Our patient empowerment program is an intensive, ten-week series of classes at our partner clinics. The program combines culturally-tailored, evidence-based diabetes education with skills training in communication and shared decision-making, a process whereby patients are equal partners in determining their treatment plans.
The goals of our patient classes are to:
- Increase patient knowledge of diabetes;
- Help patients acquire necessary skills in diabetes management;
- Support patients as they try to live healthier lives with diabetes, both in the classroom and via community resources;
- Empower patients to take a more active role with their physician in making decisions about their health care, by effectively communicating their treatment preferences and addressing barriers to shared decision-making.
The content and the structure of our classes are tailored to the needs, culture, and community of our patients.
- Our classes are shorter than many standard diabetes classes; we also meet more frequently and more often. This adaptation reduces how much information we teach per session and reinforces previously learned material.
- Audiovisual aids are important elements to the class: they address potential literacy barriers to written material. We also use interactive role-play to reinforce complex concepts (e.g., how insulin acts to regulate blood glucose levels).
- We encourage patients to share stories about their challenges and successes with managing their diabetes, and use a group format to discuss goal-setting each week. This structure builds on the oral tradition of story-telling and the religious tradition of ?testifying? in the African-American community.
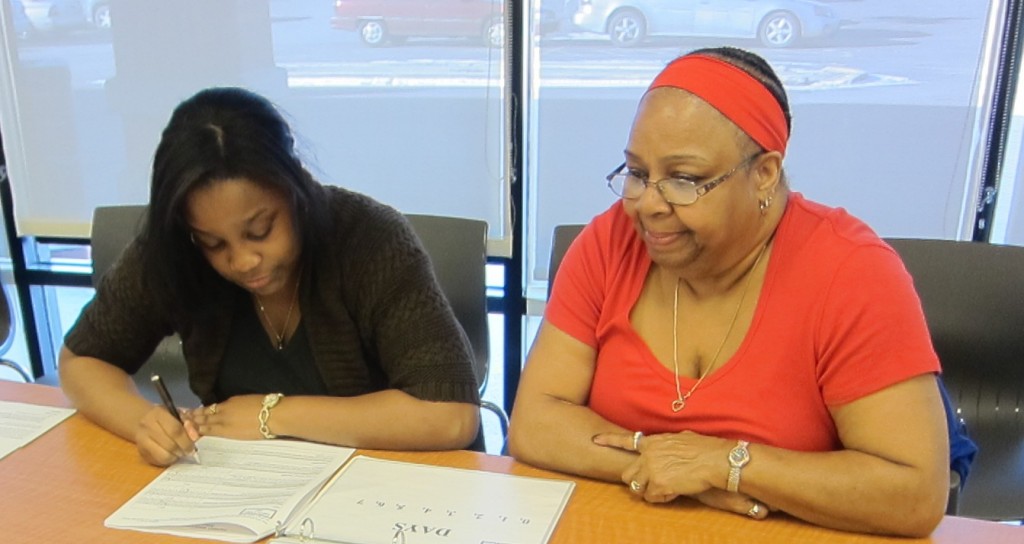
- Because of the particularly important role of family among African-Americans in health care decision-making and social support, participants are also encouraged to bring a family member or friend to the sessions to reinforce lifestyle modifications within the home and social environment.
- We address common shopping and dietary patterns in the community: for example, we created a mock grocery store with food items from a local low-cost grocer, and we use role-play to practice food ordering with local restaurant menus.
We strive to create a socially cohesive, familial environment within the class, where honest dialogue about the psychosocial challenges of diabetes is welcomed and facilitated.
Evaluating our classes
Our patients complete intensive surveys before and after the program, and every three months following, to measure self-efficacy and reported self-management behavior. We also track clinical values, specifically HbA1C, fasting lipids, blood pressure and BMI. Our preliminary results are very promising: see the relevant publications for more detail.
ÿ